Why preoperative assessment is important?
Veterinary patients presented for surgical procedures must have a preoperative medical assessment before being scheduled for surgery. This preoperative assessment of surgical patients is not only for their presenting complaints and diseases or injuries, but also for their suitability as candidates for anesthesia and the proposed surgical procedure. It indicates if further care is necessary in the perioperative period—care that could reduce the risk of surgery and the potential for postoperative complications. It helps in selecting the best procedure for the patient and prognostication, giving the clients a realistic expectation of the outcome of the proposed surgical intervention. It could also highlight other aspects of a patient’s health that may need attention and future management. It also allows a comparison of the patient’s status before and after surgery.
What are the elements of a preoperative assessment?
Preoperative assessment of surgical patients consists of a variety of elements. These are as follows:
Medical History
This is an often underrated but important part of the preoperative assessment of surgical patients. To extract the maximum benefit, medical history must be complete. A complete history can be organized in the following manner for ease of remembrance: signalment, chief/presenting complaint, history of present illness, history of past illnesses (e.g., medical, surgical, vaccinations, medications), family history (if known), environmental history, diet history and body systems review. This should be obtained from the owner or primary care giver. In an emergency, an abbreviated history is often necessary to allow emergency care to be given but does not preclude obtaining a complete history as soon as the patient is stabilized.
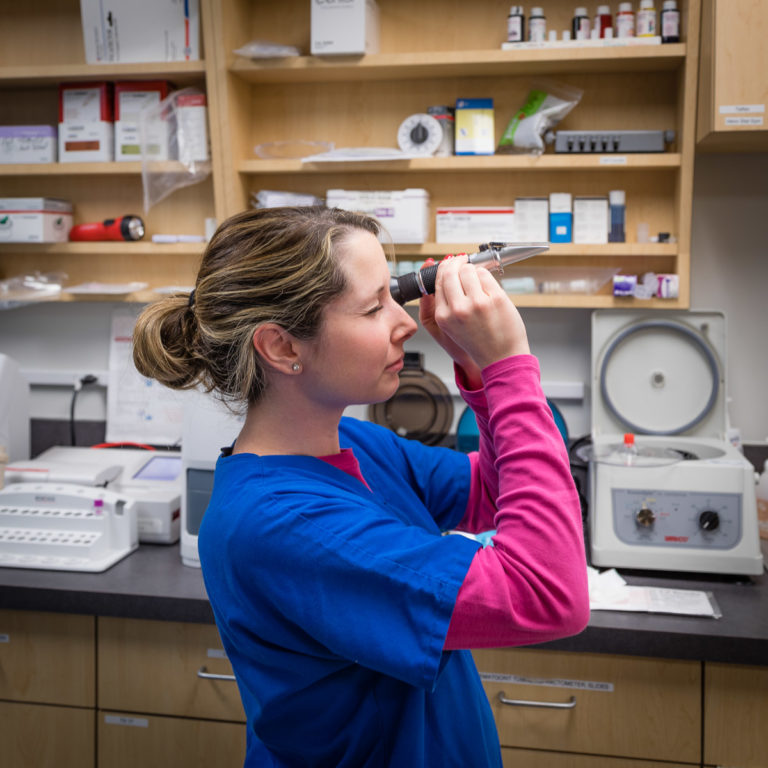
Physical Examination
Despite a natural inclination to concentrate on the presenting problems, veterinarians should focus the physical examination on evaluating the whole patient. Vital parameters and a general patient assessment, including mental status, body condition, and pain scores are a vital part of the preoperative assessment, and should be recorded. Indeed, like with medical history, a systematic approach ensures that all body systems will be evaluated.
Various formats have been described for performing a thorough physical examination. One format divides the evaluation process into examinations of the head and neck (eyes, ears, nose, and throat), forequarters, thorax, abdomen, and hindquarters. Another format emphasizes a body system approach, with the examination divided into that of the cardiovascular, respiratory, alimentary, urogenital, lymphatic, endocrine, integumentary, musculoskeletal, and neurologic systems. Note that a rectal examination is a valuable aspect of the examination and should always be performed. Whichever system is used, it is imperative for each clinician to establish his or her own pattern so it becomes a routine progression because haphazard examination always will be deficient in some category.
Physical Status
Of the procedures available for preoperative assessment, the history and physical examination described previously are most effective in detecting important abnormalities. Problems missed at this stage are usually overlooked when more invasive or expensive diagnostic tests are performed during the preoperative assessment. They also make it possible to assign a physical status to each patient, as listed in Table 1.
Physical status is a major determinant but is not a direct predictor of anesthetic or surgical risk. Rather, the major purpose of discerning physical status is to compare patients, select the most appropriate anesthetic protocol, and determine whether a patient’s status can be improved by postponing surgery in elective cases. In emergencies in which a patient’s status mandates an abbreviated examination, the physical status is qualified with an “E.” To clarify, an emergency is defined as existing when a delay in treatment would markedly increase the threat to the patient’s life or body part. In such circumstances, only data for immediate initiation of treatment are collected, and the examination is then completed after the animal is stabilized.
Table 1: Physical status in surgical patients
| Physical Status | Animal Condition | Examples |
|---|---|---|
| I | Healthy with no discernible disease. | Patient came for elective procedure (e.g., ovariohysterectomy, castration) |
| II | Healthy with localized disease or mild systemic disease that may or may not be related to the reason for surgery. | Obese but otherwise healthy patients, Neonate or Geriatric, cruciate ligament rupture, skin lump removal, controlled diabetes mellitus, mild cardiac valve insufficiency |
| III | Severe systemic disease that may or may not be related to the reason for surgery. | Pneumonia, fever, dehydration, heart murmur, anemia |
| IV | Severe systemic disease that is life threatening with or without surgery. | Heart failure, renal failure, severe hypovolemia, severe hemorrhage, sepsis, organ failure, high fever, pulmonary disease, emaciation |
| V | Moribund patient that is not expected to survive without the procedure | Severe trauma or disease that cannot be managed or mitigated prior to anesthesia and surgical procedure, Shock from ongoing severe hemorrhage, multiple organ failure |
Laboratory Data
Once a patient has been clinically evaluated, clinical problems have been identified, and a physical status has been assigned, it is possible to select laboratory tests for further preoperative assessment and evaluation. The chosen tests should be the minimum necessary to evaluate the presenting problem and its systemic manifestations and determine the significance of concurrent disease conditions detected during the initial examination. Minimum recommendations for laboratory testing based on a patient’s physical status, expected duration of surgery, and invasiveness of the planned procedure, are noted in Table 2.
Table 2: Minimum recommendations for laboratory testing.
| Physical Status | Minor Procedure (Duration <60 minutes) | Major Procedure (Duration >60 minutes or patients >7 years) |
|---|---|---|
| I | PCV, total protein, urine specific gravity. | Complete Blood Cell Count, Urinalysis, Surgical Panel (BUN, Creatinine, Alanine Aminotransferase, Alkaline Phosphatase). |
| II | PCV, total protein, urine specific gravity. | Complete Blood Cell Count, Urinalysis, Surgical Panel (BUN, Creatinine, Alanine Aminotransferase, Alkaline Phosphatase). |
| III | Complete Blood Cell Count, Urinalysis, Surgical Panel (BUN, Creatinine, Alanine Aminotransferase, Alkaline Phosphatase). | Complete Blood Cell Count, Full Biochemical Panel, Electrolyte Panel, Urinalysis |
| IV and V | Complete Blood Cell Count, Full Biochemical Panel, Electrolyte Panel, Urinalysis | Complete Blood Cell Count, Full Biochemical Panel, Electrolyte Panel, Urinalysis |
Other Diagnostic Tests
These tests can further characterize and investigate abnormalities detected during the preoperative assessment of a surgical patient. Some of these tests also can help when planning surgical procedures. (When such investigations are considered essential, but facilities do not exist, consider referring the patient.) Such tests will include some of the following:
- Coagulation studies
- Acid-base and electrolyte tests
- Organ function tests
- Hormone assays
- Plain and contrast radiography
- Electrocardiography
- Ultrasonography
- Magnetic resonance imaging
- Computed tomography
- Scintigraphy.

The essential factor in selecting tests for evaluating surgical patients is a sound understanding of the disease and its systemic effects. The procedure to be performed also influences the tests selected.
Determination of Surgical Risk
Most people know that surgical risk is a concept that weighs the relative benefits of surgery against the potential for harm. However, a much broader definition also considers the surgeon’s experience, procedure’s invasiveness, the potential for complications, and quality of the patient’s life, both with and without the recommended procedure. The overall risk is assigned once the patient has been thoroughly evaluated, and this is used in decisions about when, where, and how to proceed with surgery and other treatment plans. Occasionally, the risk of the surgical procedure may outweigh its potential benefit.
Surgical risk can determine prognosis as follows :
- Excellent: Little effect on the patient, there is minimal potential for complications, and a high probability the patient will return to normal after surgery.
- Good: High probability of a successful outcome, but the potential for complications resulting from the procedure is slightly higher than the previous category.
- Fair: One or more severe problems detected or serious complications are possible but uncommon; recovery may be prolonged, or the animal may or may not return to its presurgical function.
- Guarded: The outcome is uncertain.
- Poor: The underlying disease or surgical procedure is associated with many or severe complications; there is a significant chance of major complications, with permanent changes in general health; recovery is expected to be prolonged, and the likelihood of death during or after the procedure is high; surgery is undertaken only if a higher risk is expected if surgery is not performed (i.e., surgery is necessary to preserve life).
Client Communication
The whole purpose of the preoperative assessment of a patient is to enable the client and surgeon to make informed decisions and realize the potential for complications in the patient’s care. A thorough patient evaluation will facilitate discussions related to:
- The disease
- Its course and prognosis both with and without treatment
- Options for treatment
- Recommended procedures
- Potential complications
- Aftercare
- An estimate of the immediate and follow-up cost.
Such an understanding is not only good for the surgeon-client relationship but will also enhance clients’ compliance with recommendations for aftercare.






